XENOME: Redefining the Future of Organ Transplantation
Advancing Xenotransplantation Through Science, Ethics, and Biotechnology

Welcome to Xenome
Xenome is an integrated project in the European Sixth Framework Programme (Life Sciences, Genomics and Biotechnology for Health).
Thanks to advances in medical and technological interventions in the field of transplantation, the number of patients listed for transplants continues to rise. Currently, around 45,000 people across EU member states are waiting for various types of organ transplants. While efforts to increase organ donation, enhance the viability of sub-optimal organs, and make greater use of organs from living-related donors have made important contributions, the existing strategies are still insufficient to meet the growing demand.
To address this persistent gap, researchers are exploring multiple innovative approaches. Among the most promising are the development of artificial organs, progress in tissue engineering, and the emerging field of xenotransplantation, the transplantation of animal-derived cells, tissues, or organs into humans.
What Is Organ Transplantation?
An organ transplant is a critical and life-saving medical procedure in which a healthy organ from a donor is used to replace a patient's diseased, damaged, or failing organ. For patients with end-stage organ failure, this intervention is frequently their only course of treatment, giving them a second chance at life and greatly enhancing their quality of life.
Organs like the kidney, liver, heart, lungs, pancreas, and intestine are frequently transplanted, and tissues like corneas, skin, bone, and heart valves can also be given. Both living and deceased donors may provide transplants, especially for organs like the kidney or a portion of the liver.
Patient survival rates and transplant success have significantly increased over the past few decades due to ongoing advancements in surgical methods, immunosuppressive treatments, and post-transplant care. Nevertheless, in spite of these developments, the increasing need for transplantable organs has greatly outpaced the supply, resulting in lengthy waiting lists and, regrettably, avoidable organ shortage-related deaths.
Exploring novel and creative alternatives, such as xenotransplantation, is motivated by the pressing and continuous gap between organ supply and patient need.
What Is Xenotransplantation?
Xenotransplantation refers to any medical procedure that involves the use of living cells, tissues, or organs from one species for the benefit of another in this case, from animals to humans. It is being explored as a potential solution to the critical shortage of human donor organs, especially as demand for transplants continues to rise.
According to the most recent guidelines of the European Union, a xenotransplant is defined as any procedure that involves:
Type A Xenotransplantation
This refers to the transplantation, implantation, or infusion into a human recipient of organs, tissues, or viable cells of animal origin. In practice, this could include procedures such as transplanting a pig heart into a human patient, infusing animal-derived pancreatic islet cells to treat diabetes, or implanting animal tissues as biological scaffolds. This form of xenotransplantation is the most direct and visible, and it presents complex challenges related to immune rejection, viral safety, and physiological compatibility between species.
Type B Xenotransplantation
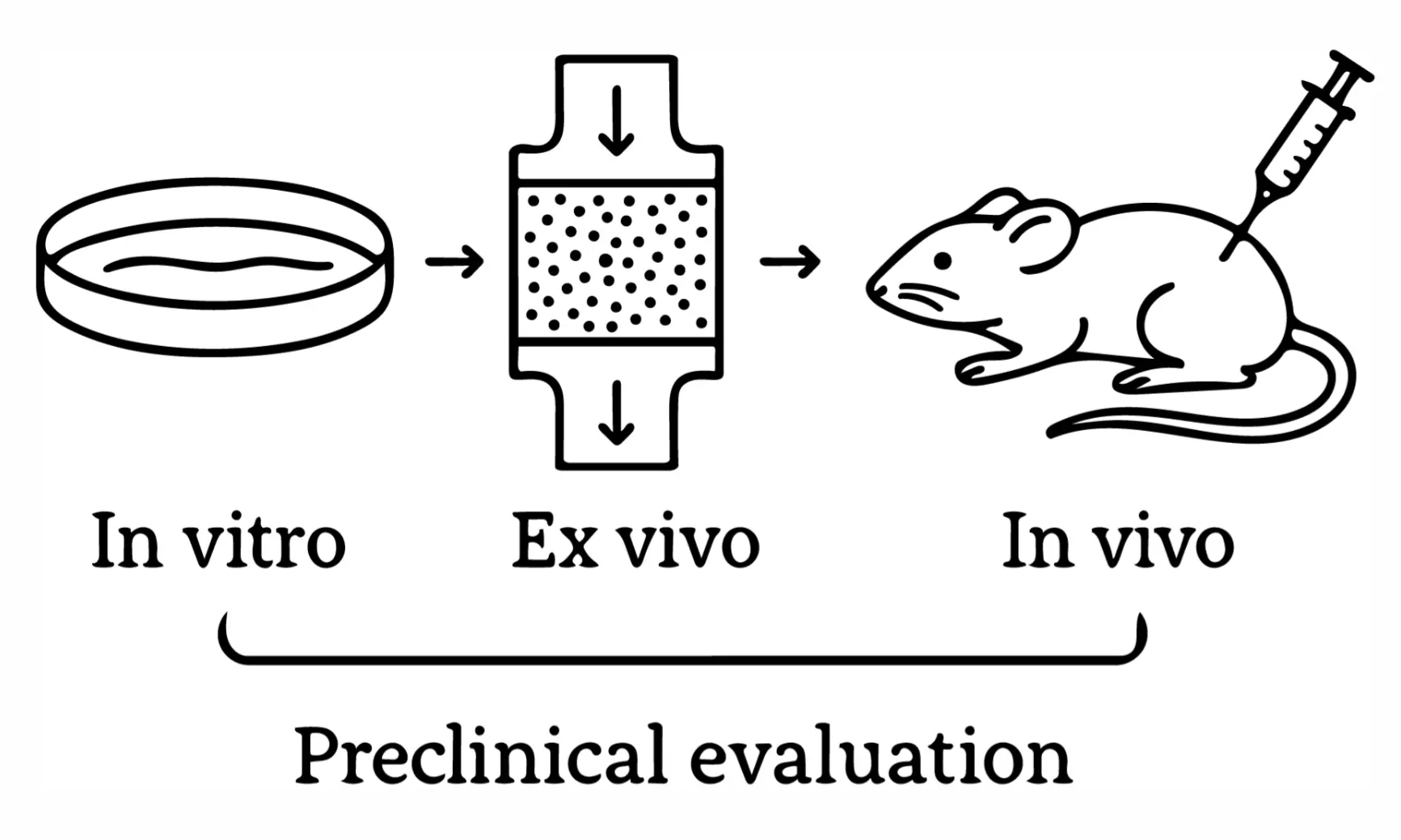
This involves the ex vivo (outside the body) contact of human body fluids, cells, tissues, or organs with live animal cells, tissues, or organs. For example, if human blood is passed through a bioartificial liver that contains living pig cells before being returned to the patient, this procedure falls under type B. While less invasive than direct transplantation, this type still carries potential risks, particularly related to cross-species infection and immune sensitization.
Biotechnology: Xenotransplantation Research
Biotechnology is at the heart of the revolution making xenotransplantation increasingly viable. Historically, the idea of transplanting animal organs or tissues into humans was hindered by insurmountable challenges particularly immune rejection, risk of cross-species infection, and incompatibility at the cellular and genetic level. Today, thanks to cutting-edge biotechnological innovations, these barriers are being actively dismantled.
Biotechnology offers a powerful suite of tools to engineer compatibility, enhance safety, and customize transplantable tissues with unprecedented precision.
Gene Editing & Genetic Engineering
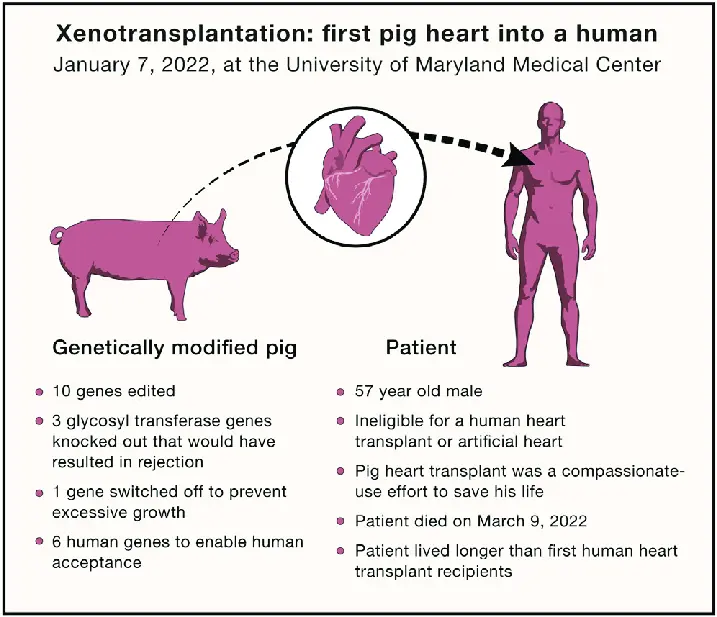
Modern gene editing technologies are revolutionizing xenotransplantation by making pig organs more compatible with the human immune system. These tools allow scientists to precisely alter the genome of donor animals, helping to reduce rejection and eliminate the risk of cross-species viral infections.
Technologies Used
CRISPR-Cas9 is the most widely used tool, enabling precise deletion or insertion of specific genes. It’s fast, accurate, and highly adaptable for multiple gene edits.
TALENs (Transcription Activator-Like Effector Nucleases) offer an alternative for targeted modifications and are often used where CRISPR is less effective.
Zinc Finger Nucleases (ZFNs) were among the first gene-editing tools and have been used to knock out specific genes in pigs, although they are now less common.
Immunomodulation & Immune Tolerance
One of the biggest challenges in xenotransplantation is the human immune system's tendency to reject foreign organs. Innovative biotechnologies are being used to modulate the immune response, allowing the body to accept animal organs
Technologies Used
Monoclonal antibodies, such as anti-CD40 and anti-CD154, are used to block key signaling pathways in the immune system. By preventing the activation of certain immune cells, these molecules help reduce aggressive responses to transplanted organs.
CAR-Treg cells (Chimeric Antigen Receptor Regulatory T cells) are specially engineered immune cells designed to promote tolerance. They can be trained to recognize the transplanted tissue and help the immune system coexist with it peacefully.
Nanoparticle-based delivery systems allow immune-modulating agents to be delivered directly to the transplant site. This localized approach enhances effectiveness while minimizing impact on the rest of the body.
Virological Safety & Screening
A critical aspect of xenotransplantation is ensuring that no viruses are passed from animals to humans. Zoonotic infections, especially those caused by porcine endogenous retroviruses (PERVs), must be carefully monitored and controlled before any clinical application.
Technologies Used
Next-Generation Sequencing (NGS) allows scientists to scan the entire genome of donor animals for hidden viral sequences. This deep-level analysis helps identify known and emerging viral threats early on.
Quantitative PCR (qPCR) is used to measure viral levels in both donor tissues and recipients. It’s a fast and sensitive tool for monitoring viral activity before and after transplantation.
Bioinformatic platforms, powered by artificial intelligence, are now being used to predict and detect viruses from large genetic datasets. These tools can flag unusual viral patterns and help assess the safety of potential donor organs.
Tissue Engineering & 3D Bioprinting
By making it possible to create hybrid organs and tissues, regenerative medicine is creating new avenues for xenotransplantation. These developments combine engineering and biology to create solutions that are better suited to the human body.
Decellularized Organs
Scientists can take a pig organ and remove all its cells, leaving behind a natural scaffold. This structure is then repopulated with human stem cells, creating a biocompatible organ that reduces the risk of rejection.
3D Bioprinting
Researchers can print intricate tissues layer by layer using specialized bio-inks derived from animal and human cells. In the future, this technology could be used to create personalized organ patches or even whole organs.








